“Blessed is the nation that doesn’t need heroes" Goethe. “Hero-worship is strongest where there is least regard for human freedom.” Herbert Spencer
Search This Blog
Showing posts with label doctor. Show all posts
Showing posts with label doctor. Show all posts
Monday 10 January 2022
Wednesday 29 December 2021
Saturday 25 September 2021
Wednesday 15 September 2021
Saturday 29 April 2017
Whiplash: the myth that funds a £20bn gravy train
Patrick Collinson in The Guardian
Ten years ago I was in a country lane in Leicestershire, indicating to turn right to go into a hotel for a family event. Seconds later my car was a write-off after a young driver careered round the bend, smashing into the rear of my VW Golf. Fortunately I stepped out uninjured. And from that moment I was pestered, again and again, to make a false whiplash claim.
One of the hotel’s guests was first in. “You’ve got to get down the doctors, tell them your neck is really hurting. You’ll easily get £3,000,” said one (I’m summarising here). But my neck, while a little stiff, wasn’t in pain. Others told me I was mad not to apply. But a decade later there is no evidence the crash caused anything other than a mild sprain that lasted a couple of days. And certainly not deserving of the £3,000-£6,000 that is routinely paid out to “victims” of even the mildest of rear-end shunts.
Now one brave consultant neurosurgeon, who has carried out thousands of operations involving neck and back issues, has declared that whiplash is a myth, nothing more than a multibillion-pound gravy train for lawyers, doctors and the victims suffering from “mainly non-existent injuries”.
In a remarkable piece for the Irish Times, Dr Charles Marks, a lecturer at University College Cork, says the medical profession is as guilty as the lawyers. “For 20 years I wrote medical reports which were economical with the truth … the truth being, there was very little wrong with the vast majority of compensation claimants that I saw. I was moving with the herd.” In Ireland, where payouts have reached levels that even the most avaricious ambulance-chasing lawyer here can only dream of, a doctor can earn as much as £3,000 a week in fees after spending 20 minutes with someone involved in a minor car crash, then writing a largely templated report. “It’s a fee of around €350 and you can easily do 10 a week,” Marks says.
Yet whiplash is “almost impossible to prove”, says Dr Marks, with patients self-diagnosing pain that can never be detected using sophisticated imaging techniques such as MRI and bone scans. “All whiplash is minor. Moderate or permanent whiplash is simply non-existent.”
He cites one study of 40 “demolition derby” drivers in the US who had an average of 1,500 collisions each over a couple of years. Compare that to a mild shunt in slow-moving traffic that, somehow, warrants payouts of thousands. Yet just two of the demolition derby drivers reported post-participation neck pain that lasted more than three months.
Dr Marks adds that in Greece and Lithuania, where there is no expectation of financial gain from whiplash, chronic neck pain following a car crash appears simply not to exist.
But one (British) consultant in Ireland is barely sufficient evidence. So I spoke to another whiplash expert, Dr Stuart Matthews, consultant surgeon in major orthopaedic trauma at the Leeds Teaching Hospitals. He sounded even more dismissive than Dr Marks. “There is not a single test that shows abnormality directly attributable to this condition. Diagnoses are purely on the say-so of the person involved. Many orthopaedic surgeons do not believe it is a genuine condition.”
He says early research that provided medical endorsement for whiplash claims has subsequently been rejected. “It’s the emperor’s new clothes. People just go along with it, there is a bandwagon.”
Neck sprain is genuine, he says, but recovery is relatively quick with little evidence of significant physical injury.
Yet the victims of whiplash receive £2bn a year in payouts, a fair chunk of which goes to personal injury lawyers. That’s £20bn over the past decade, paid for out of galloping increases in car insurance premiums. The forthcoming election means that reforms to whiplash payouts, promised in the prison and courts bill, have been shelved.
A new government, of whatever complexion, should reinstate the reforms – and order a major medical review to determine if we have all been conned for years.
Ten years ago I was in a country lane in Leicestershire, indicating to turn right to go into a hotel for a family event. Seconds later my car was a write-off after a young driver careered round the bend, smashing into the rear of my VW Golf. Fortunately I stepped out uninjured. And from that moment I was pestered, again and again, to make a false whiplash claim.
One of the hotel’s guests was first in. “You’ve got to get down the doctors, tell them your neck is really hurting. You’ll easily get £3,000,” said one (I’m summarising here). But my neck, while a little stiff, wasn’t in pain. Others told me I was mad not to apply. But a decade later there is no evidence the crash caused anything other than a mild sprain that lasted a couple of days. And certainly not deserving of the £3,000-£6,000 that is routinely paid out to “victims” of even the mildest of rear-end shunts.
Now one brave consultant neurosurgeon, who has carried out thousands of operations involving neck and back issues, has declared that whiplash is a myth, nothing more than a multibillion-pound gravy train for lawyers, doctors and the victims suffering from “mainly non-existent injuries”.
In a remarkable piece for the Irish Times, Dr Charles Marks, a lecturer at University College Cork, says the medical profession is as guilty as the lawyers. “For 20 years I wrote medical reports which were economical with the truth … the truth being, there was very little wrong with the vast majority of compensation claimants that I saw. I was moving with the herd.” In Ireland, where payouts have reached levels that even the most avaricious ambulance-chasing lawyer here can only dream of, a doctor can earn as much as £3,000 a week in fees after spending 20 minutes with someone involved in a minor car crash, then writing a largely templated report. “It’s a fee of around €350 and you can easily do 10 a week,” Marks says.
Yet whiplash is “almost impossible to prove”, says Dr Marks, with patients self-diagnosing pain that can never be detected using sophisticated imaging techniques such as MRI and bone scans. “All whiplash is minor. Moderate or permanent whiplash is simply non-existent.”
He cites one study of 40 “demolition derby” drivers in the US who had an average of 1,500 collisions each over a couple of years. Compare that to a mild shunt in slow-moving traffic that, somehow, warrants payouts of thousands. Yet just two of the demolition derby drivers reported post-participation neck pain that lasted more than three months.
Dr Marks adds that in Greece and Lithuania, where there is no expectation of financial gain from whiplash, chronic neck pain following a car crash appears simply not to exist.
But one (British) consultant in Ireland is barely sufficient evidence. So I spoke to another whiplash expert, Dr Stuart Matthews, consultant surgeon in major orthopaedic trauma at the Leeds Teaching Hospitals. He sounded even more dismissive than Dr Marks. “There is not a single test that shows abnormality directly attributable to this condition. Diagnoses are purely on the say-so of the person involved. Many orthopaedic surgeons do not believe it is a genuine condition.”
He says early research that provided medical endorsement for whiplash claims has subsequently been rejected. “It’s the emperor’s new clothes. People just go along with it, there is a bandwagon.”
Neck sprain is genuine, he says, but recovery is relatively quick with little evidence of significant physical injury.
Yet the victims of whiplash receive £2bn a year in payouts, a fair chunk of which goes to personal injury lawyers. That’s £20bn over the past decade, paid for out of galloping increases in car insurance premiums. The forthcoming election means that reforms to whiplash payouts, promised in the prison and courts bill, have been shelved.
A new government, of whatever complexion, should reinstate the reforms – and order a major medical review to determine if we have all been conned for years.
Sunday 19 June 2016
Why failure is the key to flying high

If at first you don’t succeed: Leonardo DiCaprio as Howard Hughes in The Aviator. Photograph: Miramax/Everett/Rex/Shutterstock
Matthew Syed in The Guardian
We want our children to succeed, in school and, perhaps even more importantly, in life. But the paradox is that our children can only truly succeed if they first learn how to fail. Consider the finding that world-class figure skaters fall over more often in practice than low-level figure skaters. At first sight this seems contradictory. Why are the really good skaters falling over the most?
The reason is actually quite simple. Top skaters are constantly challenging themselves in practice, attempting jumps that stretch their limitations. This is why they fall over so often, but it is precisely why they learn so fast. Shizuka Arakawa of Japan estimates that she endured some 20,000 falls as she progressed from a beginner to an Olympic champion.
Lower-level skaters have a quite different approach. They are always attempting jumps they can already do very easily, remaining within their comfort zone. This is why they don’t fall over. In a superficial sense, they look successful, because they are always on their feet. The truth, however, is that by never failing, they never progress.
What is true of skating is also true of life. James Dyson worked through 5,126 failed prototypes for his dual cyclone vacuum before coming up with the design that made his fortune. These failures were essential to the pathway of learning. As Dyson put it: “You can’t develop new technology unless you test new ideas and learn when things go wrong. Failure is essential to invention.”
Even in areas of life where failure is potentially catastrophic, it is still vital to respond positively. In aviation, for example, every aircraft is equipped with two almost-indestructible black boxes: one records the electronic information from the on-board computers and the other records sounds in the cockpit. When there is a crash, these boxes are recovered and analysed so that enlightened changes can be enacted. This means that the same mistake never happens again. It is this constant willingness to learn from failure that means aviation has become one of the world’s safest forms of transportation. Last year the accident rate for major airlines was just one crash for every 8.3 million take-offs.
In healthcare, however, things are very different. Clinicians don’t like to admit to failure, partly because they have healthy egos (particularly the senior doctors) and partly because they fear litigation. The consequence is that instead of learning from failure, healthcare often covers up failure. The direct consequence is that the same mistakes are repeated. According to the Journal of Patient Safety, 400,000 people die every year in American hospitals alone due to preventable error. That is like two jumbo jets crashing every day or 9/11 happening every few days. In the UK, too, the numbers are shocking. Until healthcare learns to respond positively to failure, things will not improve.
But let us return to children. One of the seminal mistakes in education in the 1970s was the attempt to equip children with confidence by giving them lots of successes (setting the bar very low). The consequence was that the self-esteem of kids became bound up with success, and they became unable to take risks and crumpled as soon as they hit a proper challenge.
We need to flip this approach. In a complex world, failure is inevitable. It is those individuals and institutions that have the resilience and flexibility to face up to failure, learn the lessons and adapt which ultimately excel.
Matthew Syed in The Guardian
We want our children to succeed, in school and, perhaps even more importantly, in life. But the paradox is that our children can only truly succeed if they first learn how to fail. Consider the finding that world-class figure skaters fall over more often in practice than low-level figure skaters. At first sight this seems contradictory. Why are the really good skaters falling over the most?
The reason is actually quite simple. Top skaters are constantly challenging themselves in practice, attempting jumps that stretch their limitations. This is why they fall over so often, but it is precisely why they learn so fast. Shizuka Arakawa of Japan estimates that she endured some 20,000 falls as she progressed from a beginner to an Olympic champion.
Lower-level skaters have a quite different approach. They are always attempting jumps they can already do very easily, remaining within their comfort zone. This is why they don’t fall over. In a superficial sense, they look successful, because they are always on their feet. The truth, however, is that by never failing, they never progress.
What is true of skating is also true of life. James Dyson worked through 5,126 failed prototypes for his dual cyclone vacuum before coming up with the design that made his fortune. These failures were essential to the pathway of learning. As Dyson put it: “You can’t develop new technology unless you test new ideas and learn when things go wrong. Failure is essential to invention.”
Even in areas of life where failure is potentially catastrophic, it is still vital to respond positively. In aviation, for example, every aircraft is equipped with two almost-indestructible black boxes: one records the electronic information from the on-board computers and the other records sounds in the cockpit. When there is a crash, these boxes are recovered and analysed so that enlightened changes can be enacted. This means that the same mistake never happens again. It is this constant willingness to learn from failure that means aviation has become one of the world’s safest forms of transportation. Last year the accident rate for major airlines was just one crash for every 8.3 million take-offs.
In healthcare, however, things are very different. Clinicians don’t like to admit to failure, partly because they have healthy egos (particularly the senior doctors) and partly because they fear litigation. The consequence is that instead of learning from failure, healthcare often covers up failure. The direct consequence is that the same mistakes are repeated. According to the Journal of Patient Safety, 400,000 people die every year in American hospitals alone due to preventable error. That is like two jumbo jets crashing every day or 9/11 happening every few days. In the UK, too, the numbers are shocking. Until healthcare learns to respond positively to failure, things will not improve.
But let us return to children. One of the seminal mistakes in education in the 1970s was the attempt to equip children with confidence by giving them lots of successes (setting the bar very low). The consequence was that the self-esteem of kids became bound up with success, and they became unable to take risks and crumpled as soon as they hit a proper challenge.
We need to flip this approach. In a complex world, failure is inevitable. It is those individuals and institutions that have the resilience and flexibility to face up to failure, learn the lessons and adapt which ultimately excel.
Thursday 5 May 2016
Medical Council of India similar to BCCI?
The Hindu
The Supreme Court has given the Centre a deserved rebuke by using its extraordinary powers and setting up a three-member committee headed by former Chief Justice of India R.M. Lodha to perform the statutory functions of the Medical Council of India. The government now has a year to restructure the MCI, the regulatory body for medical education and professional practice. The Centre’s approach to reforming the corruption-afflicted MCI has been wholly untenable; the Dr. Ranjit Roy Chaudhury expert committee that it set up and the Parliamentary Standing Committee on Health and Family Welfare in the Rajya Sabha had both recommended structural change through amendments to the Indian Medical Council Act. Now that the Lodha panel will steer the MCI, there is hope that key questions swept under the carpet at the council will be addressed quickly. Among the most important is the need to reduce the cost of medical education and increase access in different parts of the country. This must be done to improve the doctor-to-population ratio, which is one for every 1,674 persons, as per the parliamentary panel report, against the WHO-recommended one to 1,000. In fact, it may be even less functionally because not all registered professionals practice medicine. In reality, only people in bigger cities and towns have reasonable access to doctors and hospitals. Removing bottlenecks to starting colleges, such as conditions stipulating the possession of a vast extent of land and needlessly extensive infrastructure, will considerably rectify the imbalance, especially in under-served States. The primary criterion to set up a college should only be the availability of suitable facilities to impart quality medical education.
The development of health facilities has long been affected by a sharp asymmetry between undergraduate and postgraduate seats in medicine. There are only about 25,000 PG seats, against a capacity of 55,000 graduate seats. The Lodha committee is in a position to review this gap, and it can help the Centre expand the system, especially through not-for-profit initiatives. There is also the contentious issue of choosing a common entrance examination. Although the Supreme Court has allowed the National Eligibility-cum-Entrance Test, some States are raising genuine concerns about equity and access. A reform agenda for the MCI must include an admission procedure that eliminates multiplicity of entrance examinations and addresses issues such as the urban-rural divide and language barriers. The Centre’s lack of preparedness in this matter, even after it was deliberated by the parliamentary panel, is all too glaring. The single most important issue that the Lodha committee would have to address is corruption in medical education, in which the MCI is mired. Appointing prominent persons from various fields to a restructured council would shine the light of transparency, and save it from reverting to its image as an “exclusive club” of socially disconnected doctors.
The Supreme Court has given the Centre a deserved rebuke by using its extraordinary powers and setting up a three-member committee headed by former Chief Justice of India R.M. Lodha to perform the statutory functions of the Medical Council of India. The government now has a year to restructure the MCI, the regulatory body for medical education and professional practice. The Centre’s approach to reforming the corruption-afflicted MCI has been wholly untenable; the Dr. Ranjit Roy Chaudhury expert committee that it set up and the Parliamentary Standing Committee on Health and Family Welfare in the Rajya Sabha had both recommended structural change through amendments to the Indian Medical Council Act. Now that the Lodha panel will steer the MCI, there is hope that key questions swept under the carpet at the council will be addressed quickly. Among the most important is the need to reduce the cost of medical education and increase access in different parts of the country. This must be done to improve the doctor-to-population ratio, which is one for every 1,674 persons, as per the parliamentary panel report, against the WHO-recommended one to 1,000. In fact, it may be even less functionally because not all registered professionals practice medicine. In reality, only people in bigger cities and towns have reasonable access to doctors and hospitals. Removing bottlenecks to starting colleges, such as conditions stipulating the possession of a vast extent of land and needlessly extensive infrastructure, will considerably rectify the imbalance, especially in under-served States. The primary criterion to set up a college should only be the availability of suitable facilities to impart quality medical education.
The development of health facilities has long been affected by a sharp asymmetry between undergraduate and postgraduate seats in medicine. There are only about 25,000 PG seats, against a capacity of 55,000 graduate seats. The Lodha committee is in a position to review this gap, and it can help the Centre expand the system, especially through not-for-profit initiatives. There is also the contentious issue of choosing a common entrance examination. Although the Supreme Court has allowed the National Eligibility-cum-Entrance Test, some States are raising genuine concerns about equity and access. A reform agenda for the MCI must include an admission procedure that eliminates multiplicity of entrance examinations and addresses issues such as the urban-rural divide and language barriers. The Centre’s lack of preparedness in this matter, even after it was deliberated by the parliamentary panel, is all too glaring. The single most important issue that the Lodha committee would have to address is corruption in medical education, in which the MCI is mired. Appointing prominent persons from various fields to a restructured council would shine the light of transparency, and save it from reverting to its image as an “exclusive club” of socially disconnected doctors.
Wednesday 27 April 2016
Jeremy Hunt doesn’t understand junior doctors. He co-wrote a book on how to dismantle the NHS
Frankie Boyle in The Guardian
The health secretary’s name is so redolent of upper-class brutality he belongs in a Martin Amis book where working-class people are called Dave Rubbish

The health secretary’s name is so redolent of upper-class brutality he belongs in a Martin Amis book where working-class people are called Dave Rubbish

Jeremy Hunt: overtly ridiculous. Photograph: Mark Thomas/Rex Shutterstock
One of the worst things for doctors must be that, after seven years of study and then another decade of continuing professional exams, patients come in telling them they’re wrong after spending 20 minutes on Google. So imagine how doctors must feel about Jeremy Hunt, who hasn’t even had the decency to go on the internet.
Consider how desperate these doctors are: so desperate that they want to talk to Jeremy Hunt. Surely even Hunt’s wife would rather spend a sleepless 72 hours gazing into a cracked open ribcage than talk to him. Hunt won’t speak to the doctors, even though doctors are the people who know how hospitals work. Hunt’s only other job was founding Hotcourses magazine: his areas of expertise are how to bulletpoint a list and make dog grooming look like a viable career change.
Of course, the strikers are saying this is about safety, not pay, as expecting to be paid a decent wage for a difficult and highly skilled job is now considered selfish. Surely expecting someone to work for free while people all around them are dying of cancer is only appropriate for the early stages of The X Factor. Sadly, Tories don’t understand why someone would stay in a job for decency and love when their mother was never around long enough to find out what language the nanny spoke.
The fact that Hunt co-wrote a book about how to dismantle the NHS makes him feel like a broad stroke in a heavy-handed satire. Even the name Jeremy Hunt is so redolent of upper-class brutality that it feels like he belongs in one of those Martin Amis books where working-class people are called things like Dave Rubbish and Billy Darts (No shade, Martin – I’m just a joke writer: I envy real writers, their metaphors and similes taking off into the imagination sky like big birds or something). Indeed, Jeremy Hunt is so overtly ridiculous that he might be best thought of as a sort of rodeo clown, put there simply there to distract the enraged public.
I sympathise a little with Hunt – he was born into military aristocracy, a cousin of the Queen, went to Charterhouse, then Oxford, then into PR: trying to get him to understand the life of an overworked student nurse is like trying to get an Amazonian tree frog to understand the plot of Blade Runner. Hunt doesn’t understand the need to pay doctors – he’s part of a ruling class that doesn’t understand that the desire to cut someone open and rearrange their internal organs can come from a desire to help others, and not just because of insanity caused by hereditary syphilis.
The government believes that death rates are going up because doctors are lazy, rather than because we’ve started making disabled people work on building sites. Indeed, death rates in the NHS are going up, albeit largely among doctors. From the steel mines where child slaves gather surgical steel, all the way up to senior doctors working 36 hours on no sleep, the most healthy people in the NHS are actually the patients. This is before we get to plans for bursaries to be withdrawn from student nurses, so that we’re now essentially asking them to pay to work. Student nurses are essential; not only are they a vital part of staffing hospitals, they’re usually the only people there able to smile at a dying patient without screaming: “TAKE ME WITH YOU!”
The real reason more people die at weekends is that British people have to be really sick to stay in hospital at the weekend, as hospitals tend not to have a bar. We have a fairly low proportion of people who are doctors, don’t plan to invest in training any more, and are too racist to import them. So we’re shuffling around the doctors we do have to the weekend, when not a lot of people are admitted, from the week, when it’s busy. This is part of a conscious strategy to run the service down to a point where privatisation can be sold to the public as a way of improving things.
Naturally, things won’t actually be improved; they’ll be sold to something like Virgin Health. Virgin can’t get the toilets to work on a train from Glasgow to London, so it’s time we encouraged it to branch out into something less challenging like transplant surgery. With the rate the NHS is being privatised, it won’t be long before consultations will be done via Skype with a doctor in Bangalore. Thank God we’re raising a generation who are so comfortable getting naked online. “I’m afraid it looks like you’ve had a stroke. No, my mistake – you’re just buffering.”
When I was little, I was in hospital for a few days. The boy in the next bed was an officious little guy who took me on a tour of the ward. He’d sort of appointed himself as an auxiliary nurse and would help out around the place, tidying up the toys in the playroom, and giving all the nurses a very formal “Good Morning”, which always made me laugh. I got jelly and ice-cream one evening (I’d had my tonsils out) and they brought him some, too. Afterwards, he threw his spoon triumphantly into his plate and laughed till there were tears in his eyes. Then he tidied up and took our plates back to the trolley. What he meant by all this (we’d sit up at night talking and waiting for trains to go by in the distance) is that this was the first place he’d known any real kindness and he wished to return it. For most of us it will be the last place we know kindness. How sad that we have allowed it to fall into the hands of dreadful people who know no compassion at all, not even for themselves.
One of the worst things for doctors must be that, after seven years of study and then another decade of continuing professional exams, patients come in telling them they’re wrong after spending 20 minutes on Google. So imagine how doctors must feel about Jeremy Hunt, who hasn’t even had the decency to go on the internet.
Consider how desperate these doctors are: so desperate that they want to talk to Jeremy Hunt. Surely even Hunt’s wife would rather spend a sleepless 72 hours gazing into a cracked open ribcage than talk to him. Hunt won’t speak to the doctors, even though doctors are the people who know how hospitals work. Hunt’s only other job was founding Hotcourses magazine: his areas of expertise are how to bulletpoint a list and make dog grooming look like a viable career change.
Of course, the strikers are saying this is about safety, not pay, as expecting to be paid a decent wage for a difficult and highly skilled job is now considered selfish. Surely expecting someone to work for free while people all around them are dying of cancer is only appropriate for the early stages of The X Factor. Sadly, Tories don’t understand why someone would stay in a job for decency and love when their mother was never around long enough to find out what language the nanny spoke.
The fact that Hunt co-wrote a book about how to dismantle the NHS makes him feel like a broad stroke in a heavy-handed satire. Even the name Jeremy Hunt is so redolent of upper-class brutality that it feels like he belongs in one of those Martin Amis books where working-class people are called things like Dave Rubbish and Billy Darts (No shade, Martin – I’m just a joke writer: I envy real writers, their metaphors and similes taking off into the imagination sky like big birds or something). Indeed, Jeremy Hunt is so overtly ridiculous that he might be best thought of as a sort of rodeo clown, put there simply there to distract the enraged public.
I sympathise a little with Hunt – he was born into military aristocracy, a cousin of the Queen, went to Charterhouse, then Oxford, then into PR: trying to get him to understand the life of an overworked student nurse is like trying to get an Amazonian tree frog to understand the plot of Blade Runner. Hunt doesn’t understand the need to pay doctors – he’s part of a ruling class that doesn’t understand that the desire to cut someone open and rearrange their internal organs can come from a desire to help others, and not just because of insanity caused by hereditary syphilis.
The government believes that death rates are going up because doctors are lazy, rather than because we’ve started making disabled people work on building sites. Indeed, death rates in the NHS are going up, albeit largely among doctors. From the steel mines where child slaves gather surgical steel, all the way up to senior doctors working 36 hours on no sleep, the most healthy people in the NHS are actually the patients. This is before we get to plans for bursaries to be withdrawn from student nurses, so that we’re now essentially asking them to pay to work. Student nurses are essential; not only are they a vital part of staffing hospitals, they’re usually the only people there able to smile at a dying patient without screaming: “TAKE ME WITH YOU!”
The real reason more people die at weekends is that British people have to be really sick to stay in hospital at the weekend, as hospitals tend not to have a bar. We have a fairly low proportion of people who are doctors, don’t plan to invest in training any more, and are too racist to import them. So we’re shuffling around the doctors we do have to the weekend, when not a lot of people are admitted, from the week, when it’s busy. This is part of a conscious strategy to run the service down to a point where privatisation can be sold to the public as a way of improving things.
Naturally, things won’t actually be improved; they’ll be sold to something like Virgin Health. Virgin can’t get the toilets to work on a train from Glasgow to London, so it’s time we encouraged it to branch out into something less challenging like transplant surgery. With the rate the NHS is being privatised, it won’t be long before consultations will be done via Skype with a doctor in Bangalore. Thank God we’re raising a generation who are so comfortable getting naked online. “I’m afraid it looks like you’ve had a stroke. No, my mistake – you’re just buffering.”
When I was little, I was in hospital for a few days. The boy in the next bed was an officious little guy who took me on a tour of the ward. He’d sort of appointed himself as an auxiliary nurse and would help out around the place, tidying up the toys in the playroom, and giving all the nurses a very formal “Good Morning”, which always made me laugh. I got jelly and ice-cream one evening (I’d had my tonsils out) and they brought him some, too. Afterwards, he threw his spoon triumphantly into his plate and laughed till there were tears in his eyes. Then he tidied up and took our plates back to the trolley. What he meant by all this (we’d sit up at night talking and waiting for trains to go by in the distance) is that this was the first place he’d known any real kindness and he wished to return it. For most of us it will be the last place we know kindness. How sad that we have allowed it to fall into the hands of dreadful people who know no compassion at all, not even for themselves.
Thursday 25 February 2016
The final offer made to junior doctors was too generous – they should stop striking and get on with it
Mary Dejevsky in The Independent
You know things have reached a pretty pass in any dispute when the combatants start to invoke the spirit of deceased politicians. But when two men who have reached the top of their political trees also start invoking their own mothers – as Jeremy Corbyn and David Cameron did at Prime Minister’s Questions – well, the possibility of any agreement looks remote indeed.
Yes, after a merciful, but all too brief, period of remission, we are back in the heat of the junior doctors’ dispute. The Labour leader accused the Government of showing bad faith and “misrepresenting” statistics (about hospital deaths at weekends); the Prime Minister returned to his mantra about people not getting sick only on weekdays. Whatever else the Government may be ready to compromise on, it appears not to be a “seven-day NHS”.
And quite right, too.
“Our” NHS is not run for the benefit of the staff, however long they have spent in training, however mountainous their student loans, however arduous and responsible their work. A great many people would probably like to work only Monday to Friday, 9 to 5, especially if highly-paid overtime for additional hours comes virtually guaranteed. But this is not the reality for most people, and there is no reason, when so much in this country now functions 24/7 – with the staff on rotas and little, if any, overtime paid – why it should still be such a struggle to get the emergency services to do the same. Yet it is here the overtime culture has proved most resilient.
There will be those – and I admit to being among them – who saw the final offer to the junior doctors as too generous. By preserving a system of overtime, for Saturdays after 5pm and all Sundays, it leaves in place the idea that doctors can expect to work something like traditional office or factory hours with additional rewards for anything else. Those expectations need to be scotched.
Junior doctors, and their many vocal supporters, have tried to turn the contested statistics about weekend fatalities to their advantage, suggesting that a “cut-price” seven-day NHS would simply raise death rates around the week. Anyone who visits hospitals on weekdays and at weekends, however, will be familiar with the glaring disparity in staffing – at every level, and what sometimes appears to be a surfeit of employees, especially in the least skilled jobs, during standard working hours. There is surely money to be saved here, that could offset the cost of more staff at weekends.
Nor can the junior doctors’ dispute be seen in isolation. Their new contract is just one part – if a large part – of reform of the NHS that is yet to come. If next in line are to be the consultants, for whom the junior doctors are often deputising at nights and weekends, you can understand why the Government might be keen to hold the line.
What occasioned the latest sword-crossing in the Commons was the announcement by the British Medical Association earlier this week that the junior doctors would hold three more days of strikes, and would fight the Health Secretary’s imposition of the new contract through the courts. In the first instance, this means seeking a judicial review.
On precisely what legal grounds the BMA intends to fight is not yet clear. For all the perception that the English judiciary has become more politically engaged in recent years, it is hard to see a judge ruling that an elected government is not within its rights to set the terms of a contract for public sector employees, particular when in line with a manifesto commitment. Going to court is only going to inject more poison into this already toxic dispute.
It is beyond time that the BMA called it a day and recognised that the junior doctors have won as much as they are going to – more than they could have expected at the outset and more, indeed, than may be wise for the future health of the NHS. The BMA’s continued insistence a “safe” seven-day NHS is somehow beyond the country’s means is defeatism of the first order, and really not junior doctors’ call to make. It is the stated policy of an elected government.
That said, the extent to which this dispute has become politicised has made it infinitely harder to resolve. Jeremy Hunt has not just been defending his government’s policy of a seven-day NHS, he has been engaged directly in negotiating the small print of a new contract. This has enabled junior doctors, and the BMA on their behalf, to cast the project as a heartless Tory plot.
The most senior non-politicians – the chief executive of NHS England, Simon Stevens, and the medical director, Sir Bruce Keogh – have both been conspicuously absent from the fray. This may be because, if heads had to roll, the Health Secretary is deemed more dispensable than either of them. But here, perhaps, also lies the key to change. For 10 years or more – most recently in the Conservatives’ 2010 election manifesto – proposals have been mooted to separate the NHS from politics by placing it under an independent board. Policy, such as the creation of seven-day service, and the overall NHS budget would be set by central government, leaving the rest to professionals. Each time, however, a consensus evolved to the effect that the NHS was so integral a part of national life and the sums of money allocated so vast, that there had to be direct political accountability. The scandal at Mid-Staffs augmented that view.
But the downside of the argument is again before us. Junior doctors and a Conservative government at loggerheads; there is talk of relations blighted for a generation. One solution might be for the Government to return to its election manifesto of 2010 and divest itself of managerial responsibility for the NHS. If junior doctors can cast that as a victory, so be it. But there is no reason why the sort of hands-off arrangement that is considered good for the BBC and – increasingly – for schools should not be good for the NHS, too.
You know things have reached a pretty pass in any dispute when the combatants start to invoke the spirit of deceased politicians. But when two men who have reached the top of their political trees also start invoking their own mothers – as Jeremy Corbyn and David Cameron did at Prime Minister’s Questions – well, the possibility of any agreement looks remote indeed.
Yes, after a merciful, but all too brief, period of remission, we are back in the heat of the junior doctors’ dispute. The Labour leader accused the Government of showing bad faith and “misrepresenting” statistics (about hospital deaths at weekends); the Prime Minister returned to his mantra about people not getting sick only on weekdays. Whatever else the Government may be ready to compromise on, it appears not to be a “seven-day NHS”.
And quite right, too.
“Our” NHS is not run for the benefit of the staff, however long they have spent in training, however mountainous their student loans, however arduous and responsible their work. A great many people would probably like to work only Monday to Friday, 9 to 5, especially if highly-paid overtime for additional hours comes virtually guaranteed. But this is not the reality for most people, and there is no reason, when so much in this country now functions 24/7 – with the staff on rotas and little, if any, overtime paid – why it should still be such a struggle to get the emergency services to do the same. Yet it is here the overtime culture has proved most resilient.
There will be those – and I admit to being among them – who saw the final offer to the junior doctors as too generous. By preserving a system of overtime, for Saturdays after 5pm and all Sundays, it leaves in place the idea that doctors can expect to work something like traditional office or factory hours with additional rewards for anything else. Those expectations need to be scotched.
Junior doctors, and their many vocal supporters, have tried to turn the contested statistics about weekend fatalities to their advantage, suggesting that a “cut-price” seven-day NHS would simply raise death rates around the week. Anyone who visits hospitals on weekdays and at weekends, however, will be familiar with the glaring disparity in staffing – at every level, and what sometimes appears to be a surfeit of employees, especially in the least skilled jobs, during standard working hours. There is surely money to be saved here, that could offset the cost of more staff at weekends.
Nor can the junior doctors’ dispute be seen in isolation. Their new contract is just one part – if a large part – of reform of the NHS that is yet to come. If next in line are to be the consultants, for whom the junior doctors are often deputising at nights and weekends, you can understand why the Government might be keen to hold the line.
What occasioned the latest sword-crossing in the Commons was the announcement by the British Medical Association earlier this week that the junior doctors would hold three more days of strikes, and would fight the Health Secretary’s imposition of the new contract through the courts. In the first instance, this means seeking a judicial review.
On precisely what legal grounds the BMA intends to fight is not yet clear. For all the perception that the English judiciary has become more politically engaged in recent years, it is hard to see a judge ruling that an elected government is not within its rights to set the terms of a contract for public sector employees, particular when in line with a manifesto commitment. Going to court is only going to inject more poison into this already toxic dispute.
It is beyond time that the BMA called it a day and recognised that the junior doctors have won as much as they are going to – more than they could have expected at the outset and more, indeed, than may be wise for the future health of the NHS. The BMA’s continued insistence a “safe” seven-day NHS is somehow beyond the country’s means is defeatism of the first order, and really not junior doctors’ call to make. It is the stated policy of an elected government.
That said, the extent to which this dispute has become politicised has made it infinitely harder to resolve. Jeremy Hunt has not just been defending his government’s policy of a seven-day NHS, he has been engaged directly in negotiating the small print of a new contract. This has enabled junior doctors, and the BMA on their behalf, to cast the project as a heartless Tory plot.
The most senior non-politicians – the chief executive of NHS England, Simon Stevens, and the medical director, Sir Bruce Keogh – have both been conspicuously absent from the fray. This may be because, if heads had to roll, the Health Secretary is deemed more dispensable than either of them. But here, perhaps, also lies the key to change. For 10 years or more – most recently in the Conservatives’ 2010 election manifesto – proposals have been mooted to separate the NHS from politics by placing it under an independent board. Policy, such as the creation of seven-day service, and the overall NHS budget would be set by central government, leaving the rest to professionals. Each time, however, a consensus evolved to the effect that the NHS was so integral a part of national life and the sums of money allocated so vast, that there had to be direct political accountability. The scandal at Mid-Staffs augmented that view.
But the downside of the argument is again before us. Junior doctors and a Conservative government at loggerheads; there is talk of relations blighted for a generation. One solution might be for the Government to return to its election manifesto of 2010 and divest itself of managerial responsibility for the NHS. If junior doctors can cast that as a victory, so be it. But there is no reason why the sort of hands-off arrangement that is considered good for the BBC and – increasingly – for schools should not be good for the NHS, too.
Friday 5 February 2016
When economists ignore the human factor, we all pay the price
Timothy Garton Ash in The Guardian
Economics is not a hard science, and mathematical models won’t explain why people behave as they do. A much broader perspective is needed.
Adair Turner argued that ‘the dominant strain of academic economics and of policy-making orthodoxy’ failed to see the crisis coming. Photograph: Bloomberg via Getty Images
The Guardian recently asked nine economists whether we’re heading for another global financial crash and they gave many different answers. Yet still we turn to economists as if they were physicists, armed with scientific predictions about the behaviour of the body economic. We consumers of economics, and economists themselves, need to be more realistic about what economics can do. More modesty on both the supply and the demand side of economics will produce better results.
Following the great crash that began nearly a decade ago, there has been some soul-searching about what economics got wrong. Probably the self-criticism should have been more far-reaching, both in academia and banking, but it’s there if you look for it. In particular, the economic thinkers loosely clustered around George Soros’s Institute for New Economic Thinking (Inet) have produced a telling account of what went wrong.
Adair Turner, who saw top-level decision-making as head of Britain’s Financial Services Authority and now chairs Inet, gives a measured, cogent version of the critique in his book Between Debt and the Devil. Yes, leading academic economists did challenge the mathematical models of market perfection and, yes, financial markets may have followed oversimplistic versions of those models. Nonetheless, Turner argues, “the dominant strain of academic economics and of policy-making orthodoxy” failed to see the crisis coming, and actually contributed to it.
The key flaws were the efficient market hypothesis and the rational expectations hypothesis: economists too often assumed that market actors not only behave rationally but do so according to the same mental models deployed by economists. (Soros himself has spent a half century trying to expose this fallacy.) Modern big-picture economics (macroeconomics) also “largely ignored the operations of the financial system and in particular the role of banks”.
Market fundamentalism understood itself as the diametric opposite of the communist command economy, but in fact made the same cardinal mistake: to believe that a rational model could encompass, predict and optimise the dynamic complexity of collective human behaviour. As Roman Frydman and Michael Goldberg write: “Like a socialist planner, the economist thus believes that he can accomplish great feats, because he supposes that he has finally uncovered the fully determined mechanism which drives market outcomes.”
Large parts of academic economics fell prey to what has been called physics envy, by analogy with the Freudian notion of penis envy. Like some other areas of social science, it aspired to the status, certainty and predictability of physics. I have long thought that this hubris was fed by the fact that economics, alone among the social sciences, has a Nobel prize. Strictly speaking, it is only the Sveriges Riksbank Prize in Economic Sciences in Memory of Alfred Nobel, endowed by the Swedish central bank and first awarded in 1969, not one of the original Nobel prizes. But everyone calls it the Nobel prize. Moreover, politicians and decision-makers listen to economists in ways that they don’t, for example, listen to political scientists of the rational choice school that dominates many American university departments. This may partly be because a politician who practised rational choice politics would soon be kicked out of office, whereas the public has had to pick up the bill for those who practised rational choice economics.
This does not mean we should not pay attention to economists, nor that economics is unworthy of a Nobel prize. It just means it’s not a hard science like physics. Done properly, it takes account of culture, history, geography, institutions, individual and group psychology. John Stuart Mill said: “A man is not likely to be a good economist if he is nothing else,” and John Maynard Keynesobserved that an economist should be “mathematician, historian, statesman and philosopher in some degree”.
In another remarkable formulation, Keynes wrote: “Economics is essentially a moral science.” Indeed, one could argue that the Nobel prize for economics belongs somewhere midway between those for physics, literature and peace.Economics is, at best, a multidimensional, evidence-based craft, alert to all the influences on human behaviour, at once ambitious in scope and modest in its claims for what we can ever predict in human affairs.
What should follow from this revised, new-old understanding of the character and place of economics? I don’t know enough about university economics courses to say whether they need to adapt, but I was struck by a manifesto published a couple of years ago by economics students at Manchester University. This advocated an approach “that begins with economic phenomena and then gives students a toolkit to evaluate how well different perspectives can explain it”, rather than mathematical models based on unrealistic assumptions. (A colleague of mine claims to have heard a fierce argument between two economists in the common room of Nuffield College, Oxford, which culminated in one exclaiming to the other: “All right, assume immortality!”)
If economics is like other disciplines, it probably changes more slowly than it should, because of the strong inertial effect of older faculty personally invested in a certain way of doing the subject. Then there’s the conduct of major players, be they ministers, central bankers or business leaders. I recently read a splendidly robust lecture by the veteran investor Charlie Munger, Warren Buffett’s partner in Berkshire Hathaway, delivered in 2003, well before the crash. “Berkshire’s whole record has been achieved without paying one ounce of attention to the efficient market theory in its hard form,” he said, adding that the results of that efficient market doctrine in corporate finance “became even sillier than they were in the economics”.
Munger’s sage advice was to restore economics’ proper multidisciplinary character, not overweighting what can be counted against the unquantifiable, nor yielding to the craving for false precision, nor privileging theoretical macroeconomics over the real-life microeconomics that helped guide Berkshire’s long-term investment decisions.
We ordinary punters should learn the same lesson. We should ask of our economists, as of our doctors, only what they can deliver. There is a scientific component to medicine, larger than that in economics, but medical studies themselves indicate how much our health depends on other factors, especially psychological ones, and how much is still unknown. Economists are like doctors, only less so.
The Guardian recently asked nine economists whether we’re heading for another global financial crash and they gave many different answers. Yet still we turn to economists as if they were physicists, armed with scientific predictions about the behaviour of the body economic. We consumers of economics, and economists themselves, need to be more realistic about what economics can do. More modesty on both the supply and the demand side of economics will produce better results.
Following the great crash that began nearly a decade ago, there has been some soul-searching about what economics got wrong. Probably the self-criticism should have been more far-reaching, both in academia and banking, but it’s there if you look for it. In particular, the economic thinkers loosely clustered around George Soros’s Institute for New Economic Thinking (Inet) have produced a telling account of what went wrong.
Adair Turner, who saw top-level decision-making as head of Britain’s Financial Services Authority and now chairs Inet, gives a measured, cogent version of the critique in his book Between Debt and the Devil. Yes, leading academic economists did challenge the mathematical models of market perfection and, yes, financial markets may have followed oversimplistic versions of those models. Nonetheless, Turner argues, “the dominant strain of academic economics and of policy-making orthodoxy” failed to see the crisis coming, and actually contributed to it.
The key flaws were the efficient market hypothesis and the rational expectations hypothesis: economists too often assumed that market actors not only behave rationally but do so according to the same mental models deployed by economists. (Soros himself has spent a half century trying to expose this fallacy.) Modern big-picture economics (macroeconomics) also “largely ignored the operations of the financial system and in particular the role of banks”.
Market fundamentalism understood itself as the diametric opposite of the communist command economy, but in fact made the same cardinal mistake: to believe that a rational model could encompass, predict and optimise the dynamic complexity of collective human behaviour. As Roman Frydman and Michael Goldberg write: “Like a socialist planner, the economist thus believes that he can accomplish great feats, because he supposes that he has finally uncovered the fully determined mechanism which drives market outcomes.”
Large parts of academic economics fell prey to what has been called physics envy, by analogy with the Freudian notion of penis envy. Like some other areas of social science, it aspired to the status, certainty and predictability of physics. I have long thought that this hubris was fed by the fact that economics, alone among the social sciences, has a Nobel prize. Strictly speaking, it is only the Sveriges Riksbank Prize in Economic Sciences in Memory of Alfred Nobel, endowed by the Swedish central bank and first awarded in 1969, not one of the original Nobel prizes. But everyone calls it the Nobel prize. Moreover, politicians and decision-makers listen to economists in ways that they don’t, for example, listen to political scientists of the rational choice school that dominates many American university departments. This may partly be because a politician who practised rational choice politics would soon be kicked out of office, whereas the public has had to pick up the bill for those who practised rational choice economics.
This does not mean we should not pay attention to economists, nor that economics is unworthy of a Nobel prize. It just means it’s not a hard science like physics. Done properly, it takes account of culture, history, geography, institutions, individual and group psychology. John Stuart Mill said: “A man is not likely to be a good economist if he is nothing else,” and John Maynard Keynesobserved that an economist should be “mathematician, historian, statesman and philosopher in some degree”.
In another remarkable formulation, Keynes wrote: “Economics is essentially a moral science.” Indeed, one could argue that the Nobel prize for economics belongs somewhere midway between those for physics, literature and peace.Economics is, at best, a multidimensional, evidence-based craft, alert to all the influences on human behaviour, at once ambitious in scope and modest in its claims for what we can ever predict in human affairs.
What should follow from this revised, new-old understanding of the character and place of economics? I don’t know enough about university economics courses to say whether they need to adapt, but I was struck by a manifesto published a couple of years ago by economics students at Manchester University. This advocated an approach “that begins with economic phenomena and then gives students a toolkit to evaluate how well different perspectives can explain it”, rather than mathematical models based on unrealistic assumptions. (A colleague of mine claims to have heard a fierce argument between two economists in the common room of Nuffield College, Oxford, which culminated in one exclaiming to the other: “All right, assume immortality!”)
If economics is like other disciplines, it probably changes more slowly than it should, because of the strong inertial effect of older faculty personally invested in a certain way of doing the subject. Then there’s the conduct of major players, be they ministers, central bankers or business leaders. I recently read a splendidly robust lecture by the veteran investor Charlie Munger, Warren Buffett’s partner in Berkshire Hathaway, delivered in 2003, well before the crash. “Berkshire’s whole record has been achieved without paying one ounce of attention to the efficient market theory in its hard form,” he said, adding that the results of that efficient market doctrine in corporate finance “became even sillier than they were in the economics”.
Munger’s sage advice was to restore economics’ proper multidisciplinary character, not overweighting what can be counted against the unquantifiable, nor yielding to the craving for false precision, nor privileging theoretical macroeconomics over the real-life microeconomics that helped guide Berkshire’s long-term investment decisions.
We ordinary punters should learn the same lesson. We should ask of our economists, as of our doctors, only what they can deliver. There is a scientific component to medicine, larger than that in economics, but medical studies themselves indicate how much our health depends on other factors, especially psychological ones, and how much is still unknown. Economists are like doctors, only less so.
Tuesday 5 January 2016
By the end of my first year as a doctor, I was ready to kill myself
An Anonymous junior doctor in The Guardian
On my morning drives to the hospital, the tears fell like rain. The prospect of the next 14 hours – 8am to 10pm with not a second’s respite from the nurses’ bleeps, or the overwhelming needs of too many sick patients – was almost too much to bear. But on the late-night trips back home, I’d feel nothing at all. Deadbeat, punch-drunk, it was utter indifference that nearly killed me. Every night, on an empty dual carriageway, I had to fight with myself to keep my hands on the steering wheel. The temptation to let go – of the wheel, the patients, my miserable life – was almost irresistible. Then I’d never have to haul myself through another unfeasible day at the hospital.
By the time I neared the end of my first year as a doctor, I’d chosen the spot where I intended to kill myself. I’d bought everything I needed to do it. All my youthful enthusiasm for healing, big dreams of saving lives and of making a difference, had soured and I felt an astronomic emptiness. Made monumentally selfish by depression, I’d ceased even to care what my husband would think of me, or that my little boy would grow up without his mother.
Doctor suicide is the medical profession’s grubby little secret. Female doctors aretwice as likely as the general population to take our own lives. A US study shows our suicide rate appears higher than that of other professional groups, with young doctors at the beginning of their training being particularly vulnerable. As I wrestled silently with the urge to kill myself, another house officer in my trust went right on and did it. To me, that monstrous waste of young life seemed entirely logical. The constant, haunting fear of hurting my patients, coupled with relentless rotas at work, had rendered me incapable of reason.
Though we know large numbers of doctors kill themselves, what is less clear are the reasons why, when dedicated to preserving human life, some doctors silently plot their own deaths. A 2006 study at the University of Pennsylvania identified that during their first year as doctors, young physicians experienced skyrocketing rates of burnout, with symptoms of emotional exhaustion, depersonalisation, and reduced sense of personal accomplishment soaring from 4% to 55%.
For me, the explanation ran deeper. I was entrenched in a hospital system that brutalised young doctors. Working on my hospital’s surgical emergency unit, there were simply too few of us to cope with the daily onslaught of patients. Officially eight or 10-hour days ran routinely into 13, 14 or 15 hours as we house officers worked at fever pitch to provide what was, at best, a mediocre service for our patients. Run ragged, we fought to keep our patients safe, but their numbers outstripped ours 20 or 30 to one, and the efforts this took were superhuman. The nurses knew, the consultants knew, even the hospital management knew, yet no one seemed to give a damn.
It wasn’t just exhaustion that drove me into depression. Plenty of jobs are busy. But there is something uniquely traumatic about being responsible for patients’ lives, while being crushed under a workload so punitive it gives neither the time nor space for safe assessment of those patients. Days were bad enough, but nights on call were terrifying. I remember running from the bed of one patient, still haemorrhaging blood from her surgical wound, to another whose heart rate had plummeted to 20, perilously close to a cardiac arrest. Two stricken patients, but only one doctor, wracked with the knowledge that if something went wrong, the guilt would be hers alone.
I was lucky. I was pushed by the colleague in whom I finally confided into seeking professional help. It took anti-depressants, therapy and a narrowly-avoided psychiatric inpatient admission to bring me back to the land of the living.

Now, on the cusp of junior doctors’ first national strike in 40 years, I’m astounded the health secretary persists in ignoring unanimous condemnation of his new contract from juniors and medical leaders alike. If he gets his way, Jeremy Hunt will make it easier for hospitals to abuse their juniors, by stripping away the safeguards that stop hospitals overworking us, fining those that do. Under his new contract, our hours will become even longer, even more antisocial – at a time when we simply have nothing more to give. And as we are pushed to treat more and more patients, faster and faster, fatigue and psychological distress will dull our competence: your lives will be less safe in our hands. And our own? Take it from someone who’s been there. Watch the suicide rate climb.
On my morning drives to the hospital, the tears fell like rain. The prospect of the next 14 hours – 8am to 10pm with not a second’s respite from the nurses’ bleeps, or the overwhelming needs of too many sick patients – was almost too much to bear. But on the late-night trips back home, I’d feel nothing at all. Deadbeat, punch-drunk, it was utter indifference that nearly killed me. Every night, on an empty dual carriageway, I had to fight with myself to keep my hands on the steering wheel. The temptation to let go – of the wheel, the patients, my miserable life – was almost irresistible. Then I’d never have to haul myself through another unfeasible day at the hospital.
By the time I neared the end of my first year as a doctor, I’d chosen the spot where I intended to kill myself. I’d bought everything I needed to do it. All my youthful enthusiasm for healing, big dreams of saving lives and of making a difference, had soured and I felt an astronomic emptiness. Made monumentally selfish by depression, I’d ceased even to care what my husband would think of me, or that my little boy would grow up without his mother.
Doctor suicide is the medical profession’s grubby little secret. Female doctors aretwice as likely as the general population to take our own lives. A US study shows our suicide rate appears higher than that of other professional groups, with young doctors at the beginning of their training being particularly vulnerable. As I wrestled silently with the urge to kill myself, another house officer in my trust went right on and did it. To me, that monstrous waste of young life seemed entirely logical. The constant, haunting fear of hurting my patients, coupled with relentless rotas at work, had rendered me incapable of reason.
Though we know large numbers of doctors kill themselves, what is less clear are the reasons why, when dedicated to preserving human life, some doctors silently plot their own deaths. A 2006 study at the University of Pennsylvania identified that during their first year as doctors, young physicians experienced skyrocketing rates of burnout, with symptoms of emotional exhaustion, depersonalisation, and reduced sense of personal accomplishment soaring from 4% to 55%.
For me, the explanation ran deeper. I was entrenched in a hospital system that brutalised young doctors. Working on my hospital’s surgical emergency unit, there were simply too few of us to cope with the daily onslaught of patients. Officially eight or 10-hour days ran routinely into 13, 14 or 15 hours as we house officers worked at fever pitch to provide what was, at best, a mediocre service for our patients. Run ragged, we fought to keep our patients safe, but their numbers outstripped ours 20 or 30 to one, and the efforts this took were superhuman. The nurses knew, the consultants knew, even the hospital management knew, yet no one seemed to give a damn.
It wasn’t just exhaustion that drove me into depression. Plenty of jobs are busy. But there is something uniquely traumatic about being responsible for patients’ lives, while being crushed under a workload so punitive it gives neither the time nor space for safe assessment of those patients. Days were bad enough, but nights on call were terrifying. I remember running from the bed of one patient, still haemorrhaging blood from her surgical wound, to another whose heart rate had plummeted to 20, perilously close to a cardiac arrest. Two stricken patients, but only one doctor, wracked with the knowledge that if something went wrong, the guilt would be hers alone.
I was lucky. I was pushed by the colleague in whom I finally confided into seeking professional help. It took anti-depressants, therapy and a narrowly-avoided psychiatric inpatient admission to bring me back to the land of the living.

Now, on the cusp of junior doctors’ first national strike in 40 years, I’m astounded the health secretary persists in ignoring unanimous condemnation of his new contract from juniors and medical leaders alike. If he gets his way, Jeremy Hunt will make it easier for hospitals to abuse their juniors, by stripping away the safeguards that stop hospitals overworking us, fining those that do. Under his new contract, our hours will become even longer, even more antisocial – at a time when we simply have nothing more to give. And as we are pushed to treat more and more patients, faster and faster, fatigue and psychological distress will dull our competence: your lives will be less safe in our hands. And our own? Take it from someone who’s been there. Watch the suicide rate climb.
Tuesday 29 September 2015
‘I can’t sacrifice my family for the NHS’: the junior doctors forced out of jobs they love
Amelia Gentleman in The Guardian
At what point does a dedicated doctor, with a lifelong commitment to the NHS, decide it is time to quit? For Dr Singh, 34, a junior doctor in general medicine, the moment will come when he is no longer able to pay his mortgage and childcare bills, a situation he expects to find himself facing sometime next year.
Dr Singh has worked in hospitals, with regular A&E shifts, for 10 years since qualifying, loves his job and describes himself as “the kind of doctor you’d want to see to your gran”. But, having done an online calculation assessing how the Department of Health’s new junior doctor contract will affect his household income, he believes he and his paediatrician wife face a 25% cut to their joint take-home pay, making life in London unaffordable. He plans to move into the pharmaceutical industry.

New junior doctors' contract changes everything I signed up for
Several of Dr Singh’s friends have already left the medical profession to work as bankers and consultants in the City; others are considering emigrating to work as doctors in Australia or New Zealand. Most of them are dispirited by the proposed contract, but are more fed up with the daily stress of their work, annoyed that the long hours and considerable financial and personal sacrifices they make during their training are not appreciated, and they worry about the impact that dwindling morale could have on the NHS and its patients.
“I am not looking for parity of pay with my friends in the City. But if you can’t afford to pay your mortgage or your child’s nursery bills and you can’t look after your child yourself in the evening or [at] the weekend because the government is proposing you should work those hours on a normal basis, you can’t continue with that kind of life,” he says, asking for his full name not to be published to avoid annoying his employers. “I am a very valuable resource to the NHS. I do work incredibly hard, I really enjoy looking after my patients and I get immense satisfaction from it. I have an absolute commitment to the NHS but I can’t sacrifice my entire family for that. I have to put a roof over my son’s head.”
Junior doctors will be balloted to decide whether to strike over a radical new contract imposed on them by the Department of Health, which redefines their normal working week to include Saturday and removes overtime rates for work between 7pm and 10pm every day except Sunday. The government says the changes will come with a rise in basic salary, higher hourly rates for antisocial hours and will be “cost neutral” – but doctors believe this change could reduce salaries in some areas of medicine by up to 30%. The British Medical Association (BMA) argues that it is “unacceptable that working 9pm on a Saturday is viewed the same as working 9am on a Tuesday”.
It is unusual to hear doctors getting angry and this swell of rage is disconcerting. A social media campaign means their voices have begun to be widely heard over the past week. If the effects of the government’s austerity drive on care workers, for example, have gone largely unnoticed, the seething protest from this powerful group looks set to be harder to ignore.
Most junior doctors are smart enough to know that they will have to work hard to persuade the public that they are a genuinely needy section of society. A perception of doctors as well-paid professionals has stuck and even a semi-attentive observer knows that the harsh 100-hour-week working pattern that used to characterise medical training has been abolished.
What most people outside the medical profession are probably unaware of is that you aren’t just a junior doctor for a fleeting period after qualifying; this makes up a substantial chunk of your career – sometimes a decade, and often stretching late into your 30s. Basic salaries start at around £23,000 and are enhanced by various complicated supplements, including the antisocial hours pay that is set to be cut. Because medical training takes longer than other degrees, most junior doctors have large amounts of student debt and are expected to continue paying for the exams as part of their ongoing training, in addition to putting in large amounts of unpaid study time and paying out monthly professional payments to the General Medical Council (GMC) and the BMA.
Few people chose to go into medicine for the money, but this contract has triggered a surge of resentment about how much harder doctors work for less money than their equally ambitious and well-educated peers in other fields.
Radiologist Anushka Patchava says she will have to quit the profession if the proposals are implemented. Photograph: Teri Pengilley for the Guardian
Anushka Patchava, 29, a radiologist who qualified in 2011 and has at least two more years as a junior doctor before she graduates to being a consultant, plans to switch careers and is midway through a rigorous interviewing process with two management consultancy firms. She is fed up with the hours and the current pay and is despondent at the prospect of getting a substantial cut to her salary. She earns £31,000, which includes a 40% supplement to her basic salary, to compensate for the antisocial hours she works. Once the new contract is imposed, she thinks she will see this reduced to £27,000 or £28,000 and she expects the hours she works will become even more antisocial. She campaigned for David Cameron in May’s general election, but has subsequently rescinded her membership of the Conservative party in protest at the contract.
If she gets the management consultancy job, Patchava will quadruple her salary on day one. “It’s horrific, isn’t it?” she says. She doesn’t consider herself to be materialistic and, in normal circumstances, would not want to leave a job she loves, but the level of needless daily stress has become wearisome and she is constantly aware of lack of morale among her colleagues.
“Going into work is a struggle – you have to psych yourself up. You’re so short staffed that you can’t offer patients everything you want to offer them. There aren’t enough doctors to fill the posts that there are available now, even before the contract is brought in,” she says. “We are not supported and morale is low. You work really long hours, taking decisions that impact on people’s lives and, at the same time, you’re worrying whether your pay check is going to be enough to cover your bills.”
The daughter of two NHS surgeons, Patchava has an deep-rooted sense of loyalty to the NHS, but her parents understand the pressure she is under and why she wants to leave. There are no perks; she has to buy expensive food and coffee from the hospital cafe and pays £12 every night shift to park in the hospital car park. She calculates that, once the long hours are factored in, she earns about £10 an hour, so these costs are not negligible. As junior doctors, her parents used to get free food and free accommodation. Four of her closest friends from Cambridge, where she studied medicine, have already left to work in the City. “One of them got a gold medal in medicine, for being top of the year, but they dropped out for exactly these reasons.”
These are not alarmist stories being spread by campaigners. Even the Conservative MP and doctor Sarah Wollaston, who chairs the Health Select Committee, knows about the brain drain – her daughter has left the NHS for Australia. Now she, her husband and eight of their friends work in a hospital where they have yet to meet an Australian junior doctor in the casualty department. “It is staffed almost entirely by British-trained junior doctors,”Wollaston wrote this week.
Patchava worries about what will happen when she wants to have children and has to organise childcare for the irregular hours. Another aspect of the new contract is that parents who take time off to look after their children will no longer see their pay rise automatically while they are on leave. People who take time out of the medical training system to do research will be similarly penalised. Other changes include the removal of a supplement paid to those going into general practice, to match those working in hospitals, which doctors believe could see trainee GPs losing a third of their pay.
“I don’t have a luxury lifestyle, but I don’t think I could support children with that money and those hours,” Patchava says. “The NHS runs on the philosophy of altruism. Everyone comes in an hour early and stays late to make sure the work is done. We love the NHS, but this has been such a kick in the teeth. I’ll have no hesitation about taking a job elsewhere.”
This sense of mismatch between the commitment put in and reward taken out is widespread. “I’m 30 years old, live in a friend’s flat with three other people, don’t own a car and have still got thousands of pounds of debt,” writes one junior doctor in an angry email. “My friends outside of medicine have bought houses, have children and the majority have their weekends and evenings for themselves. On top of my ‘48 hours a week’, I teach and lecture in my free time, attend courses (which we have to fund), study and do everything I can to be a better doctor. I love my job – I couldn’t imagine living with myself if I left. However, the prevalence of locums and holes in the rota, overstretched stressed GPs and A&E staff make the atmosphere toxic. We miss weddings, funerals, birthdays. Relationships are lost, friends estranged, all because we love our job.”
Foiz Ahmed, a junior doctor in emergency plastic surgery (who is grappling with £30,000 debt) argues that the new contracts will strike a pernicious blow to the NHS and patient safety. “This isn’t just about salaries, although of course a 10-30% pay cut is unmanageable for most of us. Let’s ignore the fact that I used to earn more an hour while working for a mobile-phone company as a student ... With the continued denigration of public perception of doctors, there is a sustained attempt to make the NHS fail. A demoralised workforce performs less efficiently, and a less-efficient system can be broken up and sold to private firms.”
The Department of Heath insists these fears are misplaced. “We are not cutting the pay bill for junior doctors and want to see their basic pay go up just as average earnings are maintained. We really value the work and commitment of junior doctors, but their current contract is outdated and unfair.”
Junior doctors are not convinced. The GMC had 3,468 requests for a certificate of current professional status, the paperwork needed to register to work as a doctor outside the UK, in the 10 days since the new contract was announced; usually it processes 20 to 25 requests a day. Partly this was the result of a concerted online campaign to get junior doctors to apply as a way of showing their anger. But some doctors, such as David Watkin, 30, a paediatrician based in Birmingham, truly intend to leave if the contract is imposed. Watkin recently returned from a year working in New Zealand, has stayed in touch with his employers out there and is confident that there will be a job for him.
The day-to-day stress Watkin experiences in Birmingham, which is mainly the result of standing in for unfilled doctors’ shifts, was absent in New Zealand. “But stress is not really the issue,” he says. In New Zealand, he says he felt more looked after, with meals paid for and professional fees covered by the hospital.

Would I be a fool to return to the NHS on the new junior doctor contract?
“Here we feel very under-appreciated by the government and the Department of Health. We have sacrificed a lot – years of training and extra hours studying outside of our work. We have moved around the country every six months to go where our training jobs send us, with no say in where we go, so it’s difficult to settle anywhere and hard to buy a house. We, as a body, are feeling under attack; it feels like any concerns we raise are being misrepresented with hospitals portraying us as just wanting more money.”
At 30, he still has about £9,000 in debt (down from about £30,000). He has done seven years as a junior doctor already and has another four to go before he becomes a consultant. “I worry that this is going to lead to an exodus of doctors, and I worry about the pressure that this will put on those who stay – and on patients. I had a work-experience student with me this week; it feels harder to come out with a positive line about why they should do it.”

Holly Ni Raghallaigh: ‘I worked very hard and put myself in a lot of debt to get here.’ Photograph: Teri Pengilley for the Guardian
Holly Ni Raghallaigh, 29, a trainee urologist, is planning to go to Scotland (which, like Wales, will not impose the new contract). She has been pushed to the brink of bankruptcy by the cost of her training, and doesn’t feel able to take a pay cut. With five more years as a junior doctor, she doesn’t think she could afford to continue if her pay is reduced.
“I worked very hard and put myself in a lot of debt to get here,” she says. At one point she had to pay for a urology course ahead of an exam and was so overdrawn that she missed two consecutive monthly payments to the GMC, was temporarily removed from the medical register and subjected to a large fine. She estimates she has spent £5,000 on mandatory surgery courses and exams during surgical training; she is paying back her remaining £10,000 of student loan at a rate of £450 a month. Once her rent in London and her monthly subscriptions to the Royal College of Surgeons (£50), GMC (£40) and BMA (£18) are paid, she has nothing left. It isn’t possible to save towards a deposit on a flat.
“Every single time I found myself in my overdraft or having to borrow petrol money or forego a flight home to Ireland to book a course, or every weekend I spent working as a locum to fund my education – I would do it all over again,” she says. “I adore my job and, honestly, working in the NHS is all I have ever wanted to do. And, for the record, I am grateful to the taxpayer who has put me here.” She says she hopes the tales of difficulties she found “embarrassing and demoralising” make people understand the financial pressures junior doctors face. “I don’t want it to sound like a sob story. I could have managed my finances better, but I had no money.”
At what point does a dedicated doctor, with a lifelong commitment to the NHS, decide it is time to quit? For Dr Singh, 34, a junior doctor in general medicine, the moment will come when he is no longer able to pay his mortgage and childcare bills, a situation he expects to find himself facing sometime next year.
Dr Singh has worked in hospitals, with regular A&E shifts, for 10 years since qualifying, loves his job and describes himself as “the kind of doctor you’d want to see to your gran”. But, having done an online calculation assessing how the Department of Health’s new junior doctor contract will affect his household income, he believes he and his paediatrician wife face a 25% cut to their joint take-home pay, making life in London unaffordable. He plans to move into the pharmaceutical industry.

New junior doctors' contract changes everything I signed up for
Several of Dr Singh’s friends have already left the medical profession to work as bankers and consultants in the City; others are considering emigrating to work as doctors in Australia or New Zealand. Most of them are dispirited by the proposed contract, but are more fed up with the daily stress of their work, annoyed that the long hours and considerable financial and personal sacrifices they make during their training are not appreciated, and they worry about the impact that dwindling morale could have on the NHS and its patients.
“I am not looking for parity of pay with my friends in the City. But if you can’t afford to pay your mortgage or your child’s nursery bills and you can’t look after your child yourself in the evening or [at] the weekend because the government is proposing you should work those hours on a normal basis, you can’t continue with that kind of life,” he says, asking for his full name not to be published to avoid annoying his employers. “I am a very valuable resource to the NHS. I do work incredibly hard, I really enjoy looking after my patients and I get immense satisfaction from it. I have an absolute commitment to the NHS but I can’t sacrifice my entire family for that. I have to put a roof over my son’s head.”
Junior doctors will be balloted to decide whether to strike over a radical new contract imposed on them by the Department of Health, which redefines their normal working week to include Saturday and removes overtime rates for work between 7pm and 10pm every day except Sunday. The government says the changes will come with a rise in basic salary, higher hourly rates for antisocial hours and will be “cost neutral” – but doctors believe this change could reduce salaries in some areas of medicine by up to 30%. The British Medical Association (BMA) argues that it is “unacceptable that working 9pm on a Saturday is viewed the same as working 9am on a Tuesday”.
It is unusual to hear doctors getting angry and this swell of rage is disconcerting. A social media campaign means their voices have begun to be widely heard over the past week. If the effects of the government’s austerity drive on care workers, for example, have gone largely unnoticed, the seething protest from this powerful group looks set to be harder to ignore.
Most junior doctors are smart enough to know that they will have to work hard to persuade the public that they are a genuinely needy section of society. A perception of doctors as well-paid professionals has stuck and even a semi-attentive observer knows that the harsh 100-hour-week working pattern that used to characterise medical training has been abolished.
What most people outside the medical profession are probably unaware of is that you aren’t just a junior doctor for a fleeting period after qualifying; this makes up a substantial chunk of your career – sometimes a decade, and often stretching late into your 30s. Basic salaries start at around £23,000 and are enhanced by various complicated supplements, including the antisocial hours pay that is set to be cut. Because medical training takes longer than other degrees, most junior doctors have large amounts of student debt and are expected to continue paying for the exams as part of their ongoing training, in addition to putting in large amounts of unpaid study time and paying out monthly professional payments to the General Medical Council (GMC) and the BMA.
Few people chose to go into medicine for the money, but this contract has triggered a surge of resentment about how much harder doctors work for less money than their equally ambitious and well-educated peers in other fields.

Radiologist Anushka Patchava says she will have to quit the profession if the proposals are implemented. Photograph: Teri Pengilley for the Guardian
Anushka Patchava, 29, a radiologist who qualified in 2011 and has at least two more years as a junior doctor before she graduates to being a consultant, plans to switch careers and is midway through a rigorous interviewing process with two management consultancy firms. She is fed up with the hours and the current pay and is despondent at the prospect of getting a substantial cut to her salary. She earns £31,000, which includes a 40% supplement to her basic salary, to compensate for the antisocial hours she works. Once the new contract is imposed, she thinks she will see this reduced to £27,000 or £28,000 and she expects the hours she works will become even more antisocial. She campaigned for David Cameron in May’s general election, but has subsequently rescinded her membership of the Conservative party in protest at the contract.
If she gets the management consultancy job, Patchava will quadruple her salary on day one. “It’s horrific, isn’t it?” she says. She doesn’t consider herself to be materialistic and, in normal circumstances, would not want to leave a job she loves, but the level of needless daily stress has become wearisome and she is constantly aware of lack of morale among her colleagues.
“Going into work is a struggle – you have to psych yourself up. You’re so short staffed that you can’t offer patients everything you want to offer them. There aren’t enough doctors to fill the posts that there are available now, even before the contract is brought in,” she says. “We are not supported and morale is low. You work really long hours, taking decisions that impact on people’s lives and, at the same time, you’re worrying whether your pay check is going to be enough to cover your bills.”
The daughter of two NHS surgeons, Patchava has an deep-rooted sense of loyalty to the NHS, but her parents understand the pressure she is under and why she wants to leave. There are no perks; she has to buy expensive food and coffee from the hospital cafe and pays £12 every night shift to park in the hospital car park. She calculates that, once the long hours are factored in, she earns about £10 an hour, so these costs are not negligible. As junior doctors, her parents used to get free food and free accommodation. Four of her closest friends from Cambridge, where she studied medicine, have already left to work in the City. “One of them got a gold medal in medicine, for being top of the year, but they dropped out for exactly these reasons.”
These are not alarmist stories being spread by campaigners. Even the Conservative MP and doctor Sarah Wollaston, who chairs the Health Select Committee, knows about the brain drain – her daughter has left the NHS for Australia. Now she, her husband and eight of their friends work in a hospital where they have yet to meet an Australian junior doctor in the casualty department. “It is staffed almost entirely by British-trained junior doctors,”Wollaston wrote this week.
Patchava worries about what will happen when she wants to have children and has to organise childcare for the irregular hours. Another aspect of the new contract is that parents who take time off to look after their children will no longer see their pay rise automatically while they are on leave. People who take time out of the medical training system to do research will be similarly penalised. Other changes include the removal of a supplement paid to those going into general practice, to match those working in hospitals, which doctors believe could see trainee GPs losing a third of their pay.
“I don’t have a luxury lifestyle, but I don’t think I could support children with that money and those hours,” Patchava says. “The NHS runs on the philosophy of altruism. Everyone comes in an hour early and stays late to make sure the work is done. We love the NHS, but this has been such a kick in the teeth. I’ll have no hesitation about taking a job elsewhere.”
This sense of mismatch between the commitment put in and reward taken out is widespread. “I’m 30 years old, live in a friend’s flat with three other people, don’t own a car and have still got thousands of pounds of debt,” writes one junior doctor in an angry email. “My friends outside of medicine have bought houses, have children and the majority have their weekends and evenings for themselves. On top of my ‘48 hours a week’, I teach and lecture in my free time, attend courses (which we have to fund), study and do everything I can to be a better doctor. I love my job – I couldn’t imagine living with myself if I left. However, the prevalence of locums and holes in the rota, overstretched stressed GPs and A&E staff make the atmosphere toxic. We miss weddings, funerals, birthdays. Relationships are lost, friends estranged, all because we love our job.”
Foiz Ahmed, a junior doctor in emergency plastic surgery (who is grappling with £30,000 debt) argues that the new contracts will strike a pernicious blow to the NHS and patient safety. “This isn’t just about salaries, although of course a 10-30% pay cut is unmanageable for most of us. Let’s ignore the fact that I used to earn more an hour while working for a mobile-phone company as a student ... With the continued denigration of public perception of doctors, there is a sustained attempt to make the NHS fail. A demoralised workforce performs less efficiently, and a less-efficient system can be broken up and sold to private firms.”
The Department of Heath insists these fears are misplaced. “We are not cutting the pay bill for junior doctors and want to see their basic pay go up just as average earnings are maintained. We really value the work and commitment of junior doctors, but their current contract is outdated and unfair.”
Junior doctors are not convinced. The GMC had 3,468 requests for a certificate of current professional status, the paperwork needed to register to work as a doctor outside the UK, in the 10 days since the new contract was announced; usually it processes 20 to 25 requests a day. Partly this was the result of a concerted online campaign to get junior doctors to apply as a way of showing their anger. But some doctors, such as David Watkin, 30, a paediatrician based in Birmingham, truly intend to leave if the contract is imposed. Watkin recently returned from a year working in New Zealand, has stayed in touch with his employers out there and is confident that there will be a job for him.
The day-to-day stress Watkin experiences in Birmingham, which is mainly the result of standing in for unfilled doctors’ shifts, was absent in New Zealand. “But stress is not really the issue,” he says. In New Zealand, he says he felt more looked after, with meals paid for and professional fees covered by the hospital.

Would I be a fool to return to the NHS on the new junior doctor contract?
“Here we feel very under-appreciated by the government and the Department of Health. We have sacrificed a lot – years of training and extra hours studying outside of our work. We have moved around the country every six months to go where our training jobs send us, with no say in where we go, so it’s difficult to settle anywhere and hard to buy a house. We, as a body, are feeling under attack; it feels like any concerns we raise are being misrepresented with hospitals portraying us as just wanting more money.”
At 30, he still has about £9,000 in debt (down from about £30,000). He has done seven years as a junior doctor already and has another four to go before he becomes a consultant. “I worry that this is going to lead to an exodus of doctors, and I worry about the pressure that this will put on those who stay – and on patients. I had a work-experience student with me this week; it feels harder to come out with a positive line about why they should do it.”

Holly Ni Raghallaigh: ‘I worked very hard and put myself in a lot of debt to get here.’ Photograph: Teri Pengilley for the Guardian
Holly Ni Raghallaigh, 29, a trainee urologist, is planning to go to Scotland (which, like Wales, will not impose the new contract). She has been pushed to the brink of bankruptcy by the cost of her training, and doesn’t feel able to take a pay cut. With five more years as a junior doctor, she doesn’t think she could afford to continue if her pay is reduced.
“I worked very hard and put myself in a lot of debt to get here,” she says. At one point she had to pay for a urology course ahead of an exam and was so overdrawn that she missed two consecutive monthly payments to the GMC, was temporarily removed from the medical register and subjected to a large fine. She estimates she has spent £5,000 on mandatory surgery courses and exams during surgical training; she is paying back her remaining £10,000 of student loan at a rate of £450 a month. Once her rent in London and her monthly subscriptions to the Royal College of Surgeons (£50), GMC (£40) and BMA (£18) are paid, she has nothing left. It isn’t possible to save towards a deposit on a flat.
“Every single time I found myself in my overdraft or having to borrow petrol money or forego a flight home to Ireland to book a course, or every weekend I spent working as a locum to fund my education – I would do it all over again,” she says. “I adore my job and, honestly, working in the NHS is all I have ever wanted to do. And, for the record, I am grateful to the taxpayer who has put me here.” She says she hopes the tales of difficulties she found “embarrassing and demoralising” make people understand the financial pressures junior doctors face. “I don’t want it to sound like a sob story. I could have managed my finances better, but I had no money.”
Sunday 3 May 2015
Why all medicine men should watch Munnabhai M.B.B.S
Shuvendu Sen in The Times of India
It does not have the somber ambiance of The Doctor, where a brash MD himself succumbs to throat cancer and is hushed to humility. It does not carry the macabre interaction of a supposedly psychologically disturbed man and a tyrannical nurse as seen in One Flew Over the Cuckoo’s Nest. Neither does it inspire an awakening as Philadelphia did through a gay lawyer fighting AIDS.
Munnabhai MBBS is anything but the tempting medical plot hashing out tears, tension and hope. It walks clear of such obvious seductions. Truth be told, the movie is as loud as it can get, carries all the ingredients of Bollywood absurdity and harps on emotions, raw and running. But take a moment to peer beneath the rubble and you would smell a treasure. A rare treasure’s takes on a mission that has degenerated into a profession soaked with cynicism and slit throat parlance. And I am no film reviewer.
Let us take an earthly stand. When was the last time, we physicians have put our right hands up and taken the oath that we would take care of patients over and above vested interests? When was the last time, save glorious exceptions, we have crossed the borders of our financial gains and taken a bow for the penniless sufferer? When was the last time we thanked the hospital sweeper for his services to patient care? For that matter, when was the last time a medical book was written to highlight the absolute necessity to reach out to a stage four cancer patient other than through mindless chemotherapy and pain medications? Fact remains that medicine, like none other profession has become the yardstick of a cultivated upper lip vocation, to pursue and prevail. In our pursuit for perfection we have lost the imperfect patient.
And the fact that Munna bhai, despite all his convivial and genteel mindset, was a full blown quack, a rank outsider, drenched in liquor, roadside patois and all that was coarse and callous, made the white coat adorned messiahs look even more like bloodless bodies. Harsh words, but if anything had been flushed down the drain in the practice of medicine, it had to be empathy and emotions. Formless jottings have replaced tender words. Machines have superseded probing minds. An impatient doctor sits across the floor, rummaging the symptoms, inaccessible to the sufferer.
But of course, Munnabhai M.B.B.S has its own share of absolute lunacy. The frequent fist fights, the semi clad on-campus dance and the lugubrious antics are a far cry from the austere charm and book like precision of its western counterparts. But there’s a reason why British Medical Journal took a note of this movie. One suspects the makers of this movie played the human mind well.
Sometimes the finest sustains longer when drowned under the gross. The fine trickle beneath the plunging waves has always made its presence felt. Cure has always been the visible highpoint of medicine. It is the unseen, unspoken care that needs visibility. Munna bhai was all about that care.
Saturday 10 January 2015
Do Ched Evans or Amir have an automatic right to rehab in sport?
Kamran Abbasi in Cricinfo


The Pakistan board's unseemly haste to bring Amir back reflects poorly on it © AFP
Enlarge
Ched Evans is a footballer trying to resurrect his career. He is also a convicted rapist. Evans says he is innocent and since his release from prison he is looking for a new football team. First, he made plans to train with his old club, Sheffield United, but the public outcry was such that Sheffield United distanced themselves from him. Any subsequent opportunities with other clubs have ended abruptly following protests and threats by sponsors to end deals. Evans and his supporters argue that he deserves a chance at rehabilitation.
A few weeks ago, Ramiz Raja questioned the rush to return Mohammad Amir to professional cricket. The crimes of Amir and his fellow spot-fixers are different to that of Evans, of course, but the principle championed by Amir's supporters is the same, that he deserves a chance at rehabilitation. Ramiz spoke from the heart, of how it would feel for other players to welcome back a cheat. Pakistan's linguistic innovator has also worked as chief executive of the Pakistan Cricket Board. He speaks from board and broad experience.
Rehabilitation of offenders is an important principle that has benefits for individuals and society. No doubt that Evans and Amir and other sportsmen who commit a crime during their sporting careers have every right to be rehabilitated, but the question is whether or not they have an automatic right to be rehabilitated back into the sport they have dishonoured?
Some professions take criminal conduct so seriously that practitioners can be disbarred or struck off. The medical and legal professions are prime examples. Decisions to end careers are difficult. Professional bodies, for example the General Medical Council and the Bar Council in the United Kingdom, are responsible for making judgements on whether or not individuals are fit to practise. Hence, a barrister who has committed rape or a doctor who has made fraudulent financial claims for patient treatments will probably be judged by the relevant professional council to be unfit to remain in the profession. A doctor or barrister can be rehabilitated into society, find alternative work, but any career as a doctor or barrister will be finished.
Some professions take criminal conduct so seriously that practitioners can be disbarred or struck off. The medical and legal professions are prime examples
Society rightly demands high standards of doctors and barristers since they hold positions of influence and power. A professional sportsman is influential too, even powerful, especially in a privileged position as a role model to thousands and millions of adoring fans. Why then should a sportsman have an automatic right to return to a profession? Why shouldn't he be judged by high standards too? Role models are immensely powerful in sport and brushing over serious misdemeanours risks diminishing the gravity of the crimes. Rehabilitation back into the sport might cause offence to team-mates, fans and victims. Being disqualified from a sport might be the most powerful deterrent to future spot-fixers and rapists.
None of this reduces the onus on society and professions to support the rehabilitation of offenders. Each case requires careful consideration by a suitably qualified governing body equipped to make judgements on the seriousness of offences. But just like other professions of influence and power, rehabilitation shouldn't necessarily mean rehabilitation back into a sport. Unlike medicine and law, sport isn't geared up to make such sensitive and profound decisions. The ICC, FIFA, and national bodies like the PCB and the FA, must ensure that codes of conduct for standards of behaviour are in place and that they are enforceable.
Ramiz began to articulate that Amir and other fixers from Pakistan and elsewhere should not be rehabilitated back into professional cricket. Dissenters in England argue that Evans should not be rehabilitated back into professional football. The governing bodies of cricket and football must consider mechanisms to put the honour, reputation and values of their sports before individual and corporate gain.
This will be an unpopular view for fans who have an emotional attachment to a tainted star. Amir's case is a perfect example, tugging at our heartstrings. His role in the spot-fixing of 2010 might be judged to be too minor to bar him from cricket? But the unseemly haste to return him to international cricket reflects poorly on the PCB and ICC. A code of conduct panel for cricket might judge that other spot-fixers and match-fixers should never return to the sport. It might even decide the same for Amir?
Either way, the current systems and processes of the ICC and PCB, like the governing bodies of other sports, seem to miss the point on rehabilitation. Sport, as we are reminded each time a great player retires or moves on, is far bigger than any individual.
Tuesday 2 December 2014
Why doctors fail
Atul Gawande in the Guardian
Doctors are fallible; of course they are. So why do they find this so hard to admit, and how can they work more openly? Atul Gawande lifts the veil of secrecy in the first of his Reith lectures
Millions of moments like this occur every day: a human being coming to another human being with the body or mind’s troubles and looking for assistance. That is the central act of medicine – that moment when one human being turns to another human being for help.
And it has always struck me how small and limited that moment is. We have 13 different organ systems and at the latest count we’ve identified more than 60,000 ways that they can go awry. The body is scarily intricate, unfathomable, hard to read. We are these hidden beings inside this fleshy sack of skin and we’ve spent thousands of years trying to understand what’s going on inside. To me, the story of medicine is the story of how we deal with the incompleteness of our knowledge and the fallibility of our skills.
There was an essay that I read two decades ago that I think has influenced almost every bit of writing and research I’ve done ever since. It was by two philosophers – Samuel Gorovitz and Alasdair MacIntyre – and their subject was the nature of human fallibility. They wondered why human beings fail at anything that we set out to do. Why, for example, would a meteorologist fail to correctly predict where a hurricane was going to make landfall, or why might a doctor fail to figure out what was going on inside my son and fix it? They argued that there are two primary reasons why we might fail. The first is ignorance: we have only a limited understanding of all of the relevant physical laws and conditions that apply to any given problem or circumstance. The second reason, however, they called “ineptitude”, meaning that the knowledge exists but an individual or a group of individuals fail to apply that knowledge correctly.

We’ve relied on science to overcome ignorance, and the course of that work has itself been fascinating. That visit we made in 1995 to our paediatrician and everything that she did to sort out what was happening in my son could be traced back to 1628 when the English physician William Harvey, after millennia of ignorance, finally worked out that the heart is a pump that moves blood in a circular course through the body.
Another critical step came three centuries later, in 1929, when Werner Forssmann, a surgical intern in Eberswalde, Germany, made an observation. Forssmann was reading an obscure medical journal when he noticed an article depicting a horse in which researchers had threaded a long tube up its leg all the way into its heart. They described, to his amazement, taking blood samples from inside a living heart without harm. And he said: “Well, if we could do that to a horse, what if we did that to a human being?” Forssmann went to his superiors and said: “How about we take a tube and thread it into a human being’s heart?”
Their response was, in essence, “You’re crazy. You can’t do that. Whenever anyone touches the heart in surgery, it goes into fibrillation and the patient dies.”
He said: “Well what about in an animal?”
And they said: “There’s no point and you’re just an intern anyway. Who says you should even deserve to get to ask these questions? Go back to work.”

But Forssmann just had to give it a try. So he stole into the x-ray room, took a urinary catheter, made a slit in his own arm, threaded it up his vein and into his own heart and convinced a nurse to help him take a series of nine x-rays showing the tube inside his own heart.
He published the evidence – and was fired. Then in 1956, he was awarded the Nobel prize in medicine with André Cournand and Dickinson Richards who, some 20 years later at Columbia University, had taken Forssmann’s findings and recognised that you could not only put a catheter into the human heart but also shoot dye through the catheter. That enabled them to take pictures and see from the inside how the heart actually worked. Together the three had founded the field of cardiology. After this, doctors began devising ways to fix what was found going wrong inside the heart.
Science is concerned with universal truths, laws of how the body or the world behaves. Application, however, is concerned with the particularities, and the test of the science is how the universalities apply to the particularities. Do the general ideas about the worrying sounds the paediatrician heard in my son’s chest correspond with the unique particularities of Walker? Here Gorovitz and MacIntyre saw a third possible kind of failure. Besides ignorance, besides ineptitude, they said that there is necessary fallibility, some knowledge science can never deliver on. They went back to the example of how a given hurricane will behave when it makes landfall, how fast it will be going when it does, and what they said is that we’re asking science to do more than it can when we ask it to tell us what exactly is going on. All hurricanes follow predictable laws of behaviour but no hurricane is like any other hurricane. Each one is unique. We cannot have perfect knowledge of a hurricane, short of having a complete understanding of all the laws that describe natural processes and a complete description of the world, they said. It required, in other words, omniscience, and we can’t have that.
The interesting question, then, is how do we cope? It’s not that it’s impossible to predict anything. Some things are completely predictable. Gorovitz and MacIntyre gave the example of a random ice cube in a fire. An ice cube is so simple and so similar to other ice cubes that you can have complete assurance that if you put it in the fire, it will melt. Our puzzle is: are human beings more like hurricanes or more like ice cubes?
Following the paediatrician’s instructions, we took Walker to the emergency room. It was a Sunday morning. A nurse took an oxygen monitor, one of those finger probes with the red light, and put it on the finger of his right hand. And the oxygen level was 98%, virtually perfect. They took a chest x-ray, and it showed that the lungs were both whited out. They read it. They said: “This is pneumonia.” They did a spinal tap to make sure that it wasn’t signs of infection that had spread from meningitis. They started him on antibiotics and they called the paediatrician to let her know the diagnosis they’d found. It wasn’t the heart, they said. It was the lungs. He had pneumonia. And she said: “No, that can’t be right.” She came into the emergency room and she took one look at him – he was having trouble breathing, he was not doing great – and she saw that the finger probe with the oxygen monitor was on the wrong finger.
It turns out there are certain conditions in which the aorta can be interrupted. You can be born with an incomplete aorta and so the blood flow can come out of the heart and go to the right side of the upper body, into the hand that had that probe, but it may not go to the left side of the upper body or anywhere else. And that turned out to be what was going on. She switched the probe over to the left hand and he had an unreadable oxygen level. He was in fact going into kidney and liver failure. He was in serious trouble. She had caught a failure to apply the knowledge science has to this particular situation.
Then the team made a prediction. In this circumstance, we do have a drug – only put into use, it turned out, about a decade before my son was born: prostaglandin E2, a little molecule that can reopen the foetal circulation. When you’re a foetus in the womb, you have a bypass system that sends a separate blood supply that can stay open for a couple of weeks after birth. This system had shut down and that’s why he went into failure. But this molecule can reopen that pathway and the prediction was that this child was like every other child – that you could know what had happened to other children and could apply it here and that it would open up that foetal circulation, this bypass system. And it did. That gave him time to recover in the intensive care unit, to let his kidney and his liver recover, to let his gut start working again, and then to undergo cardiac surgery to replace his malformed aorta and to fix the holes that were present in his heart as well. They saved him.
They saved him.
There are more and more ways in which we are as knowable as ice cubes. We understand with great precision how mothers can die in childbirth, how certain tumours behave, how the Ebola virus spreads, how the heart can go wrong and be fixed. Certainly, we have many, many areas of continuing ignorance – how to stop Alzheimer’s disease or metastatic cancers, how we might make a vaccine against this virus we’re dealing with now. But the story of our time, I think, is as much a story about struggling with ineptitude as struggling with ignorance.
You go back a hundred years or more, and we lived in a world where our futures were governed largely by ignorance. But over this last century, we’ve come through an extraordinary explosion of discovery. The puzzle has, therefore, become not only how we close the gaps of ignorance open to us, but also how we ensure that the knowledge gets through, that the finger probe is on the correct finger.
Next to my son, in the intensive care unit, there was a child from Maine, which is about 200 miles away, who had virtually the same diagnosis that Walker had. And when this boy was diagnosed, it took too long for the problem to be recognised, for transportation to be arranged, and for him to get that drug to give him back that open circulation. The result was that the poor child with the same condition my son had, in the very next bed to ours, gone into complete liver and kidney failure, and his only chance was to wait for an organ transplant and hope for a future that was going to be very different from the one my son was going to have.

And then I think back on my family. My parents come from India; my father from a rural village, my mother from a big city in the north. If Walker had been anything like my nieces and nephews in the village where my family still farms – they’re farmers growing wheat and sugarcane and cotton – and if he’d been there, there would have been no chance at all.
There’s a misconception about global health. We think global health is about care in just the poorest parts of the world. But the way I think about global health, it’s about making care better everywhere – the idea that we are trying to deploy the capabilities that we have discovered over the last century, town by town, to every person alive. We’ve had an extraordinary transformation around the world. Economically, even with the last recession, we’ve had the rising of global economies on every continent and the result has been a dramatic change in the length of lives all across the world. Respiratory illness and malnutrition used to be the biggest killers. Now it’s cardiovascular disease; road traffic accidents are a top five killer and cancers are in the top 10. With economic progress has come the broader knowledge for people that solutions exist.
My family members in our village in India know that solutions exist to the problems they have, and so the puzzle is how we deploy that capability everywhere – in India, in Maine, across the UK, Europe, Latin America, the world. We’re only just discovering the patterns of how we begin to do that.
In the course of this year’s Reith lectures, I’m going to attempt to unpack three ideas. First is what we’re learning from opening the door, from seeing behind the curtains of how medicine and public health are actually practised and discovering how much can be done better that saves lives and reduces suffering. Second is the reality of our necessary fallibility and how we cope effectively with the fact that our knowledge is always limited. Third, I will consider the implications of both of these – the implications of what we’re learning about our ineptitude and about our necessary fallibility – for the global future of medicine and health.
It is uncomfortable looking inside our fallibility. We have a fear of looking. We’re like the doctors who dug up bodies in the 19th century to dissect them, in order to know what was really happening inside. We’re looking inside our systems and how they really work. And like before, what we find is messier than we knew and sometimes messier than we might have wanted to know.
In some ways, turning on the cameras inside our world can be more treacherous. There’s a reason that Gorovitz and MacIntyre labelled the kind of failures we have “ineptitude”. There’s a sense that there’s some shame or guilt attached to the fact that we don’t get it right all the time. And exposing this reality can make people more angry than exposing the reality of how the body works. Therefore, we’ve blocked many of these efforts to try to provide some transparency to what’s going on. Audiotapes are often not allowed, the video recorders are turned off. We have no black box for what happens in our operating rooms or in our clinics. The data, when we have it, is often locked up. You can’t know, even though we have the information, which hospitals have a better complication rate in certain kinds of operations than others. There’s a fear of misuse, a fear of injustice in doing it, in exposing it.
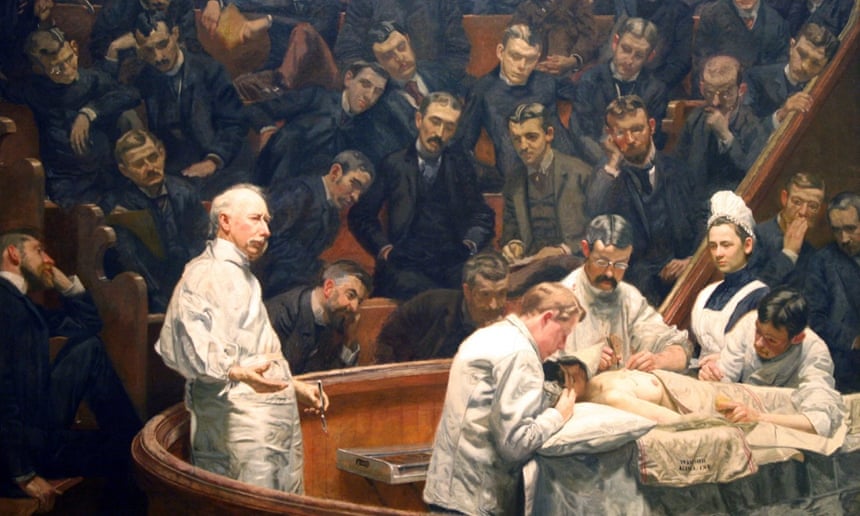
Arguably, not opening up the doors puts lives at stake. What we find out can often be miraculous. By closing ourselves off, we’re missing important opportunities.
The doctors told us when Walker went home that he was going to need a second operation. The repair that he’d had was one that replaced a section of his aorta – the tube coming out of his heart to carry blood supply throughout the rest of the body – with an artificial tube when he was 11 days old. It was almost like a straw. Now they had designed it to expand a bit as he grew, but it was not going to accommodate an adult-sized body. So they told us that when he became a teenager he would have to get a new replacement aorta and that he would have to undergo a major operation. Being a surgery resident, I knew what that entailed. Repeat aortic surgery has up to a 5% chance of death and a 25% chance of paralysis. We lived in some fear about when that moment would come.
When that moment came, he was 14 years old, and the world had changed. By then technology had developed to allow his aorta to be expanded with a simple catheter. We found the expert who had learned, and even devised, some of the methods for being able to do that, in Boston. He explained to me, cardiologist to surgeon, just how it’s done and sometimes you learn stuff you don’t necessarily want to know. He talked about how he would have to apply pressure to a balloon that would be threaded up inside the aorta. I asked how he knew what pressure to apply. He said it was by feel. He could feel the vessel tearing, and the trick was to tear it just enough that it can expand but not so much that it ruptures.
There was a necessary fallibility in what he was attempting to do – some irreducible probability of failure. But Walker got through that procedure just fine. The extraordinary thing was the very next day he went home, and the day after that he was so well that he played sports and injured his ankle on the playing field. This June he graduated from high school and this autumn he started college. He’s going to live a long and normal life, and that is amazing. The key question we have to ask ourselves is how are we going to make it possible for others to have that, how do we fulfil our duty to make it possible for others? The only way I can see is by removing the veil around what happens in that procedure room, in that clinic, in that office or that hospital. Only by making what has been invisible visible. This is why I write, this is why we do the science we do – because this is how we understand – and that is the key to the future of medicine.
Subscribe to:
Posts (Atom)
